Managing diabetes effectively involves understanding the intricate details of insulin storage and usage. One of the key questions that often arises is: “How long can insulin be out of the fridge?” This essay delves into this critical topic, addressing various sub-topics that stem from this central question, providing a comprehensive guide for those relying on insulin for diabetes management.
Insulin’s Room Temperature Stability
First and foremost, understanding the stability of insulin at room temperature is crucial. Generally, most insulins can remain effective when kept at room temperature (approximately 15-25°C or 59-77°F) for about 28 to 30 days. This time frame varies slightly depending on the type of insulin and the manufacturer’s instructions. It’s important to note that once insulin is kept at room temperature, it should not be put back in the fridge, as frequent temperature changes can degrade its quality.
Duration of Different Insulin Types Outside the Fridge
Delving deeper, it’s vital to recognize that different types of insulin have varying storage requirements. Rapid-acting, short-acting, intermediate-acting, long-acting, and pre-mixed insulins each have specific guidelines. Typically, these can be stored at room temperature for around 28 to 30 days, with some variations like insulin degludec (Tresiba) lasting up to 56 days.
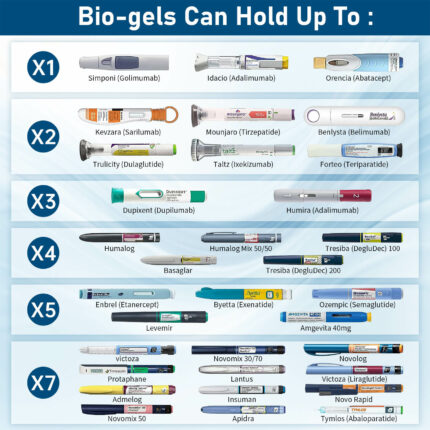
How Long Each Different Insulin Will Last Outside the Refrigerator?
Here’s a detailed overview of the typical duration various types of insulin can be kept out of the refrigerator at room temperature (around 15-25 degrees Celsius or 59-77 degrees Fahrenheit):
- Rapid-Acting Insulin:
- Examples: Insulin lispro (Humalog), insulin aspart (NovoLog), insulin glulisine (Apidra)
- Duration Out of Fridge: Generally, these can be kept at room temperature for about 28-30 days.
- Short-Acting Insulin:
- Example: Regular human insulin (Humulin R, Novolin R)
- Duration Out of Fridge: Typically, they can be used for up to 28-30 days at room temperature.
- Intermediate-Acting Insulin:
- Example: NPH insulin (Humulin N, Novolin N)
- Duration Out of Fridge: These insulins usually remain stable for up to 28-30 days at room temperature.
- Long-Acting Insulin:
- Examples: Insulin glargine (Lantus, Basaglar), insulin detemir (Levemir), insulin degludec (Tresiba)
- Duration Out of Fridge: They can often be kept out of the fridge for up to 28 days. However, insulin degludec (Tresiba) can last up to 56 days at room temperature.
- Pre-Mixed Insulin:
- Examples: NovoLog Mix 70/30, Humalog Mix 75/25, Humulin 70/30
- Duration Out of Fridge: These insulins are typically good for about 10-30 days at room temperature, depending on the specific product.
- Inhaled Insulin:
- Example: Afrezza
- Duration Out of Fridge: Once opened, the cartridge is usually good for up to 10 days at room temperature.
- Insulin Pens and Cartridges:
- For most insulin pens and cartridges, the room temperature stability is similar to that of vials, which is typically about 28-30 days.
It’s important to note that these durations can vary based on factors like brand, specific formulation, and manufacturing. Additionally, always visually inspect the insulin for any changes in appearance (such as discoloration or crystallization) before use, regardless of the time out of the fridge.
Always refer to the specific product’s packaging or consult with a healthcare professional for the most accurate and up-to-date information regarding storage and handling for your particular insulin.
Why Insulin Shouldn’t Be Put Back in the Fridge
The question, “Why can’t insulin be put back in the refrigerator after it has been kept at room temperature?” addresses a common concern. The key reason is to avoid temperature fluctuations which can cause insulin degradation. Proteins like insulin are sensitive to such changes, and it’s recommended to follow the manufacturer’s guidelines for optimal storage.
Insulin’s Appearance and Efficacy
Addressing “Why does insulin become cloudy at room temperature?” and related concerns, it’s essential to understand that not all insulin is designed to be clear. Insulin types like NPH are naturally cloudy, but if a typically clear insulin becomes cloudy, this could indicate a problem like contamination or exposure to adverse conditions, leading to reduced efficacy.
Why Does Insulin Become Cloudy at Room Temperature?
Insulin can become cloudy at room temperature due to various reasons, and it’s important to understand that not all types of insulin are meant to be clear. Here’s a detailed explanation:
- Types of Insulin: There are different types of insulin, and their appearance can vary. Rapid-acting and long-acting insulins are usually clear, while intermediate-acting insulins (such as NPH insulin) and some pre-mixed insulins are intentionally cloudy. The cloudiness in these insulins is due to the addition of certain substances that slow the insulin’s absorption, prolonging its duration of action.
- Protein Aggregation: Insulin is a protein, and at certain temperatures or after a period of time, proteins can aggregate or come together. This aggregation can cause the insulin to appear cloudy or to form precipitates. This is more common in insulin that has been stored improperly (like being exposed to extreme temperatures) or is past its expiration date.
- Suspension Insulins: Some insulins are formulated as suspensions, where the insulin is suspended in a liquid but not completely dissolved. These insulins need to be mixed gently before use. If not mixed properly, they can appear unevenly cloudy or have clumps.
- Temperature Changes: Repeated temperature changes can affect insulin stability. For instance, moving insulin repeatedly between cold and room temperatures might cause changes in its appearance, including cloudiness.
- Contamination or Deterioration: If insulin is contaminated or has deteriorated, it may appear cloudy. Contamination can occur if the insulin is handled improperly or if the vial or pen is left open for extended periods.
- Insulin Zn Formulation: Some insulins, especially older formulations, contain zinc, which helps to stabilize the insulin and control its release. Changes in temperature can affect the zinc-insulin complex, potentially leading to cloudiness.
It’s crucial to understand that for some insulin types, such as NPH, the cloudiness is normal and expected. However, if a typically clear insulin appears cloudy or if there are visible particles or color changes in any insulin, it should not be used. In all cases, it’s important to follow storage instructions and regularly inspect insulin for any changes in appearance. If in doubt, consult with a healthcare professional for guidance.
Can I use insulin after it becomes cloudy?
Whether you can use insulin after it becomes cloudy depends on the type of insulin and the reason for the cloudiness. Here’s a detailed explanation:
Insulin Designed to be Cloudy: Some insulin types, such as NPH (Neutral Protamine Hagedorn) or certain pre-mixed insulins, are naturally cloudy. This cloudiness is due to the addition of protamine or other agents that slow down the absorption of insulin, making it intermediate- or long-acting. In these cases, the cloudiness is normal, and the insulin should be gently rolled or inverted to mix it before use.
Clear Insulin Turning Cloudy: If a type of insulin that is supposed to be clear (like rapid-acting or long-acting insulin) becomes cloudy, this can indicate a problem. Causes may include contamination, exposure to extreme temperatures, or expiration. Using insulin that has become cloudy when it’s supposed to be clear can be risky because the insulin might have lost its potency or could be contaminated.
Risk of Ineffective Insulin: If insulin is cloudy due to degradation or improper storage, using it can lead to ineffective blood sugar control. Insulin that has changed in appearance may not lower blood glucose levels as expected, which can lead to high blood sugar (hyperglycemia) or unpredictable blood sugar fluctuations.
Potential for Contamination: Cloudiness can also indicate contamination, which can be harmful. Injecting contaminated insulin can lead to infections or other complications at the injection site.
Manufacturer’s Guidelines: Always follow the manufacturer’s guidelines for the specific type of insulin you are using. These guidelines provide information on how the insulin should appear and what to do if there are changes in its appearance.
Consulting Healthcare Professionals: If you’re unsure about the insulin’s appearance or its safety, consult a healthcare professional before using it. They can provide guidance and help you determine whether the insulin is safe to use.
In summary, for insulin types that are meant to be cloudy, such as NPH and some pre-mixed insulins, cloudiness is normal after mixing. However, if an insulin that should be clear becomes cloudy, or if there are any other changes in the appearance of any insulin, it’s best to err on the side of caution and consult a healthcare professional before using it.
Why can’t insulin be put back in the refrigerator after it has been kept at room temperature?
Insulin can often be stored at room temperature after it’s been removed from the refrigerator to make injections more comfortable, as cold insulin can be painful to inject. However, there’s a common misconception that once insulin is kept at room temperature, it shouldn’t be put back in the fridge. Let’s clarify this:
- Temperature Fluctuations: Frequent changes in temperature can potentially degrade the insulin. Proteins, like insulin, can be sensitive to environmental conditions. Moving insulin back and forth between the fridge and room temperature could cause it to break down or lose efficacy more quickly.
- Stability at Room Temperature: Most modern insulins are formulated to be stable at room temperature (about 15-25°C or 59-77°F) for a certain period (commonly 28-30 days) once they are opened. This stability is based on the assumption that the insulin will be kept consistently at room temperature.
- Risk of Condensation: When insulin is moved from a colder environment (like a fridge) to a warmer one, condensation can occur inside the vial or cartridge. This moisture can potentially affect the concentration and purity of the insulin, leading to less effective or unpredictable blood glucose control.
- Manufacturer’s Guidelines: The stability and storage instructions for insulin are based on extensive testing by the manufacturer. These guidelines are meant to ensure the insulin maintains its efficacy until its expiration date. It’s always best to follow these guidelines, which usually include instructions on whether the insulin can be refrigerated again after being kept at room temperature.
- Practical Considerations: In practice, many people do return their insulin to the fridge after using it at room temperature without apparent issues. The key is to avoid extreme or frequent temperature changes and not to use insulin past its room temperature expiration date.
- Consulting Healthcare Professionals: If you’re unsure about the best way to store your insulin, it’s advisable to consult with a healthcare professional or the insulin manufacturer for guidance.
In summary, while insulin may not necessarily be harmed by being refrigerated again after being at room temperature, it’s generally recommended to avoid frequent temperature changes to maintain its stability and effectiveness. Always follow the storage guidelines provided by the insulin manufacturer and consult healthcare professionals for personalized advice.
Insulin Exposure to Environmental Conditions
Another vital aspect to consider is why insulin should be kept out of direct sunlight. Sunlight exposes insulin to heat and UV light, which can lead to the degradation of the insulin molecule, affecting its ability to regulate blood sugar effectively. Maintaining insulin in a controlled environment away from extreme conditions is key to preserving its efficacy.
What happen when insulin left out of fridge for 2 or 12 hours
Leaving insulin out of the fridge for short periods like 2 hours or even 12 hours generally does not compromise its efficacy, provided it is kept under appropriate conditions. The stability and safety of insulin in these scenarios depend on several factors:
Insulin Left Out for 2 Hours
- Room Temperature Stability: Modern insulin formulations are typically stable at room temperature (15-25°C or 59-77°F) for much longer than 2 hours. This stability is designed to accommodate daily use patterns.
- No Significant Degradation: At room temperature, insulin doesn’t undergo significant degradation within such a short period. Therefore, it remains effective for managing blood glucose levels.
- Convenience and Comfort: Many individuals prefer to inject insulin at room temperature as cold insulin can be uncomfortable. Leaving it out for a short period like 2 hours is often done for this reason.
Insulin Left Out for 12 Hours
- Still Within Safe Range: For most types of insulin, being out of the fridge for 12 hours is typically within the safe range, as long as the insulin is not exposed to extreme temperatures or direct sunlight.
- Manufacturer’s Guidelines: It’s important to refer to the insulin’s storage instructions. Most insulins can remain effective for up to 28-30 days at room temperature once opened.
- Visual Inspection: After 12 hours, it’s advisable to inspect the insulin for any changes (like cloudiness in clear insulin types, or color changes). If it appears normal, it is generally safe to use.
If you need to be out for an extended period, you should consider preparing a portable insulin cooler to prevent the insulin from spoiling.
General Considerations
- Avoid Extreme Conditions: Insulin should always be kept away from direct sunlight, heat sources, and freezing temperatures, regardless of the duration it’s left out.
- Repeated Exposure: Regularly leaving insulin out for extended periods or exposing it to fluctuating temperatures could potentially affect its stability over time.
- Consult Healthcare Professionals: If unsure about the insulin’s integrity after being left out, it’s best to consult a healthcare professional.
In summary, insulin left out of the fridge for 2 or 12 hours is unlikely to be harmful if kept under recommended conditions. However, it’s crucial to follow storage guidelines provided by the manufacturer and to inspect the insulin before use.
Short-Term Exposure: Insulin Outside the Fridge
Exploring scenarios like “What happens when insulin is left out of the fridge for 2 hours” or for “12 hours,” it’s noted that short-term exposure to room temperature generally does not harm insulin. However, it should still be stored in a safe environment, away from extreme heat or sunlight. Most insulins can tolerate such short durations out of refrigeration without losing potency, but caution and adherence to manufacturer guidelines are advised.
Conclusion
In conclusion, understanding how long insulin can be out of the fridge is fundamental for anyone managing diabetes. This essay has explored various facets of insulin storage, from its room temperature stability to the effects of environmental exposure. By adhering to manufacturer guidelines and being mindful of storage conditions, individuals can ensure that their insulin remains effective, thus maintaining optimal diabetes management.